Background:
Cytomegalovirus (CMV) serostatus is associated with transplant related mortality, relapse and survival following allogeneic stem cell transplant (SCT). Prior studies have demonstrated that CMV seronegative recipients (R-) receiving a CMV seropositive graft (D+) experience inferior outcomes compared to the R-/D- combination, an observation that is independent of viral reactivation and due to increased bacterial and fungal sepsis (Nichols WG et al, J. Infect. Dis. 2002; 185:273-82). We therefore investigated the hypothesis that CMV exposure, including that by the donor only prior to transplant, promotes endogenous and long-term immunodeficiency after SCT.
Methods:
A total of 108 patient peripheral blood samples were obtained from the Chronic Graft-vs.-Disease (GVHD) Consortium, which includes both patients with and without chronic GVHD. Seventy-three baseline samples were taken at an average of 458 days (range 63 to 1,965) after SCT, and 35 paired blood samples were taken at an average of 94 days follow-up. Transplant parameters, CMV serostatus, and CMV viral titers after SCT were collected. We performed multiparameter flow cytometry to assess innate and adaptive immunity after SCT in the context of CMV, including transcription factor and cytokine expression, together with TCR/BCR sequencing to assess immune diversity.
Results:
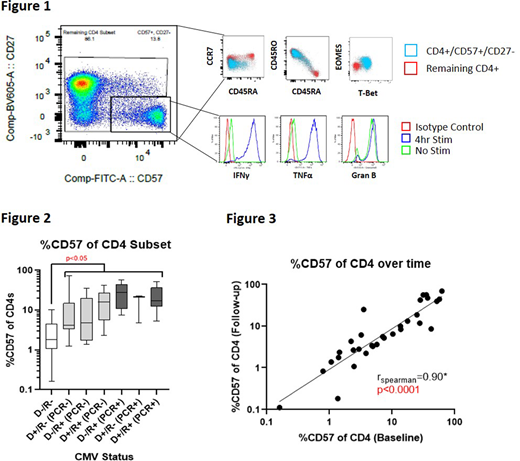
We demonstrate that CMV exposure (including solely in the donor prior to transplant or in the recipient after transplant) is strongly associated with long-lasting expansion of a terminally differentiated MHC class II-restricted donor memory T cell subset identifiable by the surface markers CD4+/CD57+/CD27-(Figure 1). These cells are CCR7neg/CD45RO+/CD45RA+/-, express T-bet, eomesodermin (EOMES), granzyme B, and secret high amounts of Th1 cytokines IFNγ and TNF (Figure 1). This T cell subset represents an average of 2.8% for D-/R- transplants and >10% (and up to 70%) of total CD4+ T cells in all other serostatus combinations irrespective of the presence or absence of measurable CMV reactivation after SCT (p<0.05 across all pairwise comparisons with D-/R- subset, Figure 2). Furthermore, this phenotype persists in an expanded fashion for years following SCT (samples were taken up to 5 years post-SCT). Follow-up samples from the same patient taken up to 218 days after the initial sample confirm phenotypic stability over time (r=0.90, p<0.0001, Figure 3). Detectable CMV replication after SCT further augmented this memory CD4+ T cell subset, and antiviral treatment for CMV did not limit its expansion. We demonstrate that these differentiated memory CD4+ T cells are associated with a significant loss of T cell receptor diversity (r=-0.60, p=0.004) and reduced proportions of major histocompatibility class (MHC) II expressing classical monocytes (r=-0.43, p=0.0002) and plasmacytoid dendritic cells (r=-0.31, p=0.0085) in peripheral blood.
Conclusion:
These data describe a temporally stable, expanded MHC class II-restricted memory T cell population with high cytotoxic potential and putative mechanisms by which CMV exposure modifies immune function in the peri-transplant period, namely the limitation of TCR diversity and antigen presentation. This cell population is expanded even in the absence of detectable CMV reactivation post SCT and can be observed for several years following transplant. We thus provide a potential mechanism for the immunodeficiency and broad increase in infection mortality invoked by CMV exposure. In particular, these findings may provide a rationale for supporting the selection of CMV- donors for R- SCT recipients.
Jagasia:Ocugen: Other; Mallinckrodt: Research Funding; Janssen: Research Funding. Dahlman:Kadmon Holdings, Inc: Other. Lee:Syndax: Research Funding; Pfizer: Consultancy, Research Funding; AstraZeneca: Research Funding; Amgen: Research Funding; Kadmon: Research Funding; Takeda: Research Funding; Novartis: Research Funding; Incyte: Consultancy, Research Funding. Hill:Generon: Consultancy; Roche: Research Funding; Compass Pharmaceuticals: Research Funding; CSL: Research Funding; Implicit Bioscience: Research Funding; Pharmacyclics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal